The CoPilot VL®
It has finally arrived. The next generation of video intubation tools is here, and I got my hands on one of the first.
So were do I get the CoPilot VL®?
| Learn more about the CoPilot VL for EMS at Medsouth1.com |
 |
It has finally arrived. The next generation of video intubation tools is here, and I got my hands on one of the first.
| Learn more about the CoPilot VL for EMS at Medsouth1.com |
 |
Tags:gear, intubation, patient care
Posted in EMS Stuff Reviewed, Featured, slider | 3 Comments »

It has finally arrived. The next generation of video intubation tools is here, and I got my hands on one of the first.
1st generation video scopes
Five years ago the EMS world was introduced to the GlideScope. This mythological end all tool was only whispered about by most EMS providers due to the 15K price tag. What the GlideScope did was simply put a video camera on a laryngoscope and a separate view screen . The idea here was that in a difficult airway situation were getting a direct view of the anatomy was difficult or near impossible we had a camera to guide us. This was quite revolutionary and everyone wanted one.
Next came the competition. Some versions were a simple redesign at a lower price while others made modifications such as including the view screen on the handle of the scope. These first generation video scopes all have one thing in common, the actual process of intubating was the same as before.
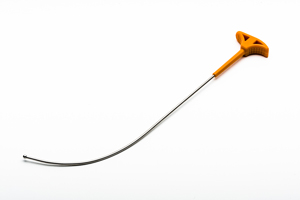
Next up, the CoPilot VL® (video laryngoscope)
the first and only generation 2 video laryngoscope.

After you are finished intubating there is a button on the handle of the scope that releases the blade into the bio bag. Grab slide another blade on and you are ready to go. No cleaning of this equipment unless it was a truly messed up call. So I guess there is no need for all those autoclaves in our stations, LOL.
The other accessories include a power cord, IV pole clamp, and a handy bag. The unit will run for 2 hours before you need to plug it in. You could intubate every patient in a shift before you need to recharge. The IV clamp will probably end up in the EMS junk drawer. This was intended for hospital use.
The CoPilot VL® was not a redesign of previous units but a redesign of the intubation process addressing the known issues.
The curvature of the blade on the CoPilot VL® is set perfectly. You simply drop the blade and you are looking right up at the cords. Slide your Bougie down the port, click click click and your in. It really is that simple.
No matter how revolutionary and cool a new tool is there is one main factor that will be a deal breaker and that is price. Most of us working the ambulance have never seen a GlideScope in real life due to the $15,000 price tag. However the CoPilot VL® is nicely priced at $2999.00. The disposable blades will run you $10.00 each.
No need to remove a C-Collar / no more manipulating anatomy
Absolutely. This company carries the slogan “First time, every time”. I do believe it. You really have to use it only once to see just how easy it makes intubation. Even an EMT-Basic can do it. (LOL just kidding guys)
First time, every time
| Learn more about the CoPilot VL for EMS at Medsouth1.com |
 |
Tags:gear, intubation, patient care, productivity
Posted in EMS Stuff Reviewed, Featured, slider | 2 Comments »
 In this edition of The Other Side of EMS we head down south to the Gulf coast during a hurricane to find out what to expect when you volunteer for storm duty.
In this edition of The Other Side of EMS we head down south to the Gulf coast during a hurricane to find out what to expect when you volunteer for storm duty.
I have worked in north central Louisiana for 8 years now and have been deployed to 4 different storms. I have taken part in hurricanes Dean, Katrina, Gustav and now Isaac. Each deployment was a unique experience with completely different mission tasks. The main advice I can give anyone traveling down here to help out is to not expect anything and to plan for everything.
My Hurricane Isaac Response video – all clips in this video are my own.
Plan to be gone from 1 to 2 weeks. Every deployment we are told to expect to be gone for a week but every time it is extended to at least 2 weeks. Keep this in mind if you have medications. With the loss of power or flooding pharmacies are not open and usually have delays getting shipments even after the lights come back on. During Katrina and Isaac we found ourselves sleeping in the truck for 2 or 3 nights so a blanket and pillow is a must. Although its impractical bringing insulin and dry baby formula would have made a massive difference in Katrina. The military dropped plenty of MREs to the crowd but the babies were hungry too.
Bring your cell phone. Hurricanes have a tendancy to take out communications and you can’t tell which forms will still work. During Hurricane Katrina cell towers as well as radio towers went down. We were pretty much left with our truck to truck radios. I think the cellular providers have since taken steps to prevent this. Even as the power went out in Belle Chasse during Isaac Verizon’s towers never faltered. I can’t say the same for AT&T and even the state radios we were issued.
Finding diesel for the trucks WILL be a problem when the storm hits and maybe for a few days after. In Belle Chasse there was one brave gas station that stayed open on generator power, at least until it caught on fire. Be sure to fill your tank up at every opportunity. In a pinch find military personel, they can help find you some. If all else fails find a truck and a garden hose, you are in fact in a state of emergency.
 When your unit deploys to Louisiana your first stop will be to register with the Louisiana Bureau of EMS, this will be your governing body for the duration. The registration location is usually located at the bureau’s office in Baton Rouge however during Hurricane Gustav this was further north in Alexandria. You will not only be registering everyone in your group but also your ambulance and your equipment. To expedite things your team leader needs to have a packet ready on each person to include copies of drivers licenses, copies of certification cards and cell phone number.
When your unit deploys to Louisiana your first stop will be to register with the Louisiana Bureau of EMS, this will be your governing body for the duration. The registration location is usually located at the bureau’s office in Baton Rouge however during Hurricane Gustav this was further north in Alexandria. You will not only be registering everyone in your group but also your ambulance and your equipment. To expedite things your team leader needs to have a packet ready on each person to include copies of drivers licenses, copies of certification cards and cell phone number.
In addition to the crew packets you can speed things up by having your stretcher serial number, yes there is one, and monitor serial number ready, although they may want to actually see these. Each team will be issued a state 700 radio that you must protect with your life. Each unit will be given an id number to tape to your windshield. From this point out you receive your orders from the bureau and your team will likely leave the building with your first mission. This is where things get unpredictable. Your missions can range from manning a Red Cross shelter, evacuation of a nursing home, or to assist with an overwhelmed 911 system.
 Sometimes in extreme situations your mission might be to assist with a forward hospital or rescue collection point.
Sometimes in extreme situations your mission might be to assist with a forward hospital or rescue collection point.
At Hurricane Katrina our team arrived in Baton Rouge the day prior to landfall ridding out the storm at the bureau. When it was safe to travel south into New Orleans we did so at slow pace. Our mission was to reach the dome and setup triage and treatment. 12 hours later we arrived at the dome. To my surprise we were the first medical crews there. We established triage and treatment areas on the back loading docks.
During the night we triaged around 1500 people as they arrived by helicopter, military trucks and by foot. We soon got word that no transports would be leaving for the next 24 to 48 hours. This presented new problems. There were patients that needed dialysis including emergency dialysis, diabetic patients that had been without insulin for days, and patients on ventilators. Imagine running a hospital with only the stuff from the ambulance. The rules we are used to were no longer valid. A new triage color was created, blue. This was for the patients that would normally be red but we could not help. The blue patients were not expected to make it through the night.
One volunteer single handedly saved the lives of 2 blue patients. She sat in a chair in between the 2 vent patients and bagged them both all night long.
There was one exception, one person did get transported out that night. A woman in labor came through triage. She was 9 months pregnant, grav 4 para 3, all had to be c-sectioned. We managed to get the military to fly her out that night. By morning the flood waters began to rise and we were pulled out of the dome.
At no other time in my ems career was the phrase adapt and overcome more true.
 Most evacuations occur prior to the storm making landfall. During Hurricane Gustav we teamed up with Acadian Ambulance and helped evacuate nursing homes. One or two bed bound patients in the back and fill the rest up with the ambulatory. Usually these patients would be taken a few hours away to another facility. Any evacuations that are done after this point will be in an emergent fashion.
Most evacuations occur prior to the storm making landfall. During Hurricane Gustav we teamed up with Acadian Ambulance and helped evacuate nursing homes. One or two bed bound patients in the back and fill the rest up with the ambulatory. Usually these patients would be taken a few hours away to another facility. Any evacuations that are done after this point will be in an emergent fashion.
During the storm facilities can be damaged or flooded causing the need for emergency evacuation. A tornado spun off of Gustav and struck a hospital during the night so we convoyed in and loaded there patients up.
Katrina was so underestimated that evacuation missions made up the majority ems activities. After being pulled from the Super Dome we went straight to were the interstate dipped below the flood water to receive bed bound patients from Tulane Hospital that would arrive by boat. We loaded up our patients and drove straight to Baton Rouge dropping them off at the LSU Pete Maravich Assembly Center (The P-MAC). The rest of my time at Katrina was evacuating people from New Orleans, most would come from evacuation points and other facilities including Baptist Memorial.
Every Red Cross Shelter must have ems present. Most larger shelters or any shelter with special needs patients will have a treatment area manned by ems. This was one of our primary missions during Isaac. Plaquemines Parish had 3 shelters set up in Belle Chasse which is 10 minutes south of New Orleans. We arrived before the storm hit and would stay in Belle Chasse for the next two weeks.
 There is not much to do at a small shelter. Ours had maybe 20 people. Luckily I still have an unlimited data plan on my phone and Verizon does not throttle because I stayed on Netflix.
There is not much to do at a small shelter. Ours had maybe 20 people. Luckily I still have an unlimited data plan on my phone and Verizon does not throttle because I stayed on Netflix.
Our other primary mission was to integrate with Plaquemines Parish EMS and run 911 calls. Being right on the coast Plaquemines call volume tends to increase with any hurricane. After the storm we were needed even more than before. They lost units to flood waters and some of there crews were isolated, cut off by flooding.
Other units from our company were stationed in New Orleans and other locations helping with their 911.
 Hurricane Katrina was a good bad experience, if that makes sense. I am glad I went but it left me with a little PTSD. I never understood exactly what that was until then.
Hurricane Katrina was a good bad experience, if that makes sense. I am glad I went but it left me with a little PTSD. I never understood exactly what that was until then.
After being pulled from the Super Dome and waiting on the patients to arrive by boat from Tulane I was staring off into the flooded city when an old man leaned over and said “if you stare into that water long enough you will see them bodies”. That was when I realized the magnitude of Katrina was more than I had expected.
A lady walked up with a can of dry baby formula. She had no way to open the can and no water to mix it with. I managed to open the can and give her plenty of water. I wanted to tell her to get in for a ride to Baton Rouge.
On another day we were stationed on top of a bridge near the dome waiting to enter the Garden District to evacuate Baptist Memorial when a couple approached with an infant that had just died. It was obvious that the cause was dehydration due to the sweltering heat and lack of water. A horrible effect of underestimating a hurricane.
Once cleared to enter the Garden District we proceeded to into the neighborhood when one of our units was shot at. We stopped while our police escorts raced forward and dealt with the situation. We arrived at the corner of St. Charles and Napoleon St. were there was a Rite Aid being looted by local residences and police. I know what you are thinking but hold on and hear me out. The police officer was breaking into the pharmacy to help a resident get seizure meds for his mother who had already seized multiple times. The rest of the people were mainly after anything to drink, water, fruit punch, Dr Pepper, or whatever. At this point looting a store was done for survival not greed. Its a shame officers got in trouble doing this, they had no supplies either. A large number of people arrived by boat to be evacuated and we didn’t have enough trucks for them all, or so we thought. That run we took 11 people packed tightly into our type 2 ambulance.
The situation had deteriorated to the point that staying and treating patients did no good. The only effective action we could take to save lives was to get as many people out of New Orleans as possible and that is what we did.
 From then on we made trip after trip taking people to Baton Rouge. Each time the ride into New Orleans became more stomach turning and the ride back more somber and exhaustive. My wife, who was my partner, and I would reflect on the days events and I could tell it was taking its toll on her. People were dying waiting to leave the city and it all could have been avoided. On night 7 after the storm we arrived at the PMAC with a load of patients and were greeted by a lady asking if we had any children without parents. I will never forget that. The situation had actually deteriorated to that point. I looked at my wife who was holding back tears and told her it was time to go home and hug our kids.
From then on we made trip after trip taking people to Baton Rouge. Each time the ride into New Orleans became more stomach turning and the ride back more somber and exhaustive. My wife, who was my partner, and I would reflect on the days events and I could tell it was taking its toll on her. People were dying waiting to leave the city and it all could have been avoided. On night 7 after the storm we arrived at the PMAC with a load of patients and were greeted by a lady asking if we had any children without parents. I will never forget that. The situation had actually deteriorated to that point. I looked at my wife who was holding back tears and told her it was time to go home and hug our kids.
It was another 2 weeks before we could get back on the truck. Our company did a debrief a few days later that really helped. It would be another 7 years before I went back to the Big Easy but only because Hurricane Isaac was bearing down.
Katrina for me was a rough and stressful deployment that left me jaded but I am glad I went.

 A hurricane deployment is a good experience and will show you just how versatile an EMS system can become.
A hurricane deployment is a good experience and will show you just how versatile an EMS system can become.
I usually enjoy any ems activity that will get me off of the truck for awhile, not that I don’t like working on the ambulance but its always good to change it up.
During the storm can be fun, just sit back and enjoy or play some football.
One last plus is the fact that FEMA pays very well.
I encourage you to come on down and help out if given the opportunity. Whether you have a good experience or a bad one during your deployment to a hurricane it will be one of the highlights of your ems career that you will tell your grandkids about.
Katrina Response video – clips taken from youtube


Tags:around the world, gustav, hurricane, isaac, katrina
Posted in slider, The Other Side of EMS | Comments Closed

The Other Side of EMS is a series highlighting the many different EMS systems that are not the typical ambulance on the street setup.In this edition of The Other Side of EMS I talked to Jeffrey Armstrong who gave me look behind the scenes of Walt Disney World’s EMS system.
The task of providing emergency medical services to the 70,000 people per park at Walt Disney World is contracted to Reedy Creek Emergency Services (RCES). This fire department based service was created in 1968 to provide emergency services to Walt Disney World. RCES’s response personnel are certified by the State of Florida as Firefighters, Emergency Medical Technicians, Fire Safety Inspectors, and Paramedics.

There are 4 fire stations located in the district, which by the way are the nicest and coolest looking stations I have ever seen. Each station has 4 engines, a tower truck, two 4 x 4 brush trucks, a specialized squad truck, a tanker and 7 ALS ambulances. In addition, the department has a special 6 x 6 aerial ladder designed to service the monorail beam in off-road areas.
In 1971, RCES began its delivery of emergency medical services (EMS) to the employees and guests of Walt Disney World. Initially, this service was two-fold. EMS was provided through response to the areas within the District and to provide industrial medical services to the employees of Walt Disney World after the close of their first-aid facilities. In 1976 the Department began the delivery of ALS Paramedic Services within the District. Today, 24-hour shift personnel working out of four fire stations staffing 7 in-service ALS transport units deliver this service. The EMS system is under the medical control of the Orange County Medical Director.

In 2001, Emergency Services implemented a program know as MARC, Medical Assistance Response Cart, to reduce response times. These customized golf carts are the first response to any 911 call placed within the park. According to my wife these are the cutest little ambulances ever. These compact units are fully stocked with some of the best equipment including the electric Stryker stretcher and Lifepak 12 monitor. These carts are able to receive call information via a mounted computer.
The MARC personnel work 8, 10, or 12 hour shifts depending on the need and consist of 24 Paramedics and EMT’s and are not required to be certified Firefighters.
MARC personnel also provide CPR and other medical related training programs to the Walt Disney employees.

There are 6 MARC stations located through out the parks. 1 station per park except Epcot which has 2. Magic Kingdom has 1 station with 2 units. Each MARC unit runs an average of 10 – 14 calls per shift.
The MARC teams are the first response to any 911 medical call. The team will quickly arrive at the patient, evaluate and begin treating. If transport is needed the team will call for one of the 7 ambulances within the parks to transport. The MARC team does not leave the park with the patient.
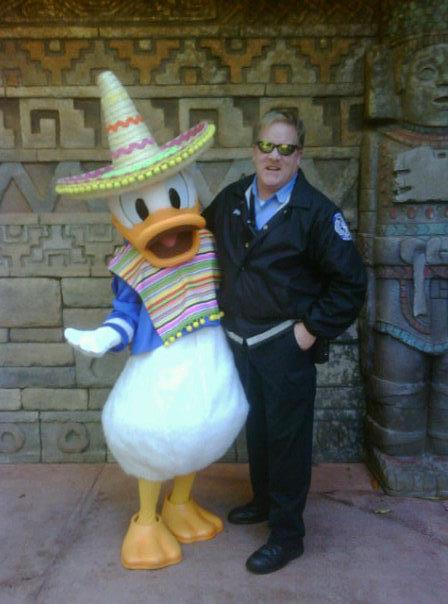 Jeffrey Armstrong is an EMT of 18 years and works full time as a MARC team member. To Jeff working as an EMT in the Walt Disney parks is more like an adventure than a job. Everyday Jeff meets and treats people from all walks of life and backgrounds. There are no ‘frequent fliers’ as there are in most systems. But what most of his patients do have in common is their chief complaint, or actually the reason for their chief complaint. Walt Disney World is located in Florida and if you have visited any of the southern states you know that the summer heat and humidity can be brutal. As you would guess Jeff treats many patients with heat injuries but a larger number of patients have pre existing conditions that are exacerbated by the heat. One other unique patient care hazard to EMS at Walt Disney World is the all mighty dollar. No, not what Disney charges the patient for EMS care, in fact that service is free of charge, but these patients have spent $5,000 or more on this vacation and they flat out do not want to go to the hospital. Jeff says a big part of patient interaction is convincing the patient to go to the hospital. The summer months are definitely the busiest being described as ‘organized chaos’ were Jeff stays busy running back to back calls. There are slow days that these medics enjoy, rain days. While other services would see a rise in calls such as MVAs crews at Disney get to enjoy a little down time.
Jeffrey Armstrong is an EMT of 18 years and works full time as a MARC team member. To Jeff working as an EMT in the Walt Disney parks is more like an adventure than a job. Everyday Jeff meets and treats people from all walks of life and backgrounds. There are no ‘frequent fliers’ as there are in most systems. But what most of his patients do have in common is their chief complaint, or actually the reason for their chief complaint. Walt Disney World is located in Florida and if you have visited any of the southern states you know that the summer heat and humidity can be brutal. As you would guess Jeff treats many patients with heat injuries but a larger number of patients have pre existing conditions that are exacerbated by the heat. One other unique patient care hazard to EMS at Walt Disney World is the all mighty dollar. No, not what Disney charges the patient for EMS care, in fact that service is free of charge, but these patients have spent $5,000 or more on this vacation and they flat out do not want to go to the hospital. Jeff says a big part of patient interaction is convincing the patient to go to the hospital. The summer months are definitely the busiest being described as ‘organized chaos’ were Jeff stays busy running back to back calls. There are slow days that these medics enjoy, rain days. While other services would see a rise in calls such as MVAs crews at Disney get to enjoy a little down time.
Working for RCES at Disney also comes with a few benefits. Even though they are not employed by Disney they do enjoy the discounts and privileges. To get an idea of what it is like everyday just follow @JEFF_EMT on twitter. Here are a few tweets from Jeff.
“I am finer than frog hair #myEMSday will be hanging with pre star wars weekends people here at Disney hollywood studios.”
“best part of job #myEMSday to find interesting ways take pictures of #Epcot fireworks.”
“Worth the wait #myemsday (@ Wishes! Nighttime Fireworks Spectacular w/ 12 others) “
“just started #myEMSday adventure for today here magic kingdom.hoping the EMS Gods are good to me today.”
“Just another day here in paradise #myemsday (@ Reedy Creek Emergency Services Medic 12 at Disney Hollywood Studios)”
I think this last one would best sum up how Jeff views his job at the happiest place on earth.
Tags:around the world, employment
Posted in slider, The Other Side of EMS | 2 Comments »
The first question that must be answered before accepting a patient’s refusal is whether or not the patient can refuse. Most of the time this is simple enough but there are some special considerations that if addressed and documented will give added protection to the provider and ems agency in court.
As with any other patient we assess we want to know if the patient’s mental status is altered. In addition to determining if the patient is alert and oriented x4, especially when dealing with a possible head injury or intoxicated patient, we need to ensure the patient’s short term memory is intact by asking the patient to remember three items. Before accepting the refusal have the patient repeat these things back to you. Court cases have shown that this level of assessment does not quite finish the job. The patient’s level of awareness needs to be further evaluated.
The courts want to know if the paramedics determined that the patient actually knew what was going on and was able to make an informed decision.
The patient needs to understand the nature of the condition and risks of refusing care as well as the benefits of being evaluated at the ED. This step can be easily determined. Inform the patient of the condition and describe the risks of refusing care as well as the benefits to being evaluated in an emergency room which should include abilities of the ED that you can not perform such as labs and CT. Ask the patient to repeat this back to you in his own words. This demonstrates that the patient is aware of the situation and possible outcomes. If the patient can not do this then you should continue patient care under implied consent. If the patient does pass these tests, even with ETOH on board, then the patient has the right to refuse care.
Practical Tip: EXPLOIT uncertainty! Many patients are unsure about whether or not to go to the hospital, and that uncertainty can be used to your advantage in advising the patient to obtain the care they need.
The advise in this section is intended for those working in states that do not have laws that address refusals and intoxicated patients. Not having laws to protect the provider means that we should take extra care to avoid a lawsuit. Research your local laws to determine just how covered you are.
When dealing with a possibly drunk patient think of their mental status as either being altered or not. The odor of ETOH alone does not mean the patient can no longer refuse care. If you suspect the patient to be intoxicated but not altered then keep these caveats in mind.
The final draft of our protocol addresses the possibly intoxicated patient. Specific criteria are outlined that if any are true then assume implied consent to treat and transport, utilizing the police if needed.
You are called to the home of an elderly female with hip pain. The family tells you they have a signed power of attorney and want her transported. The patient however flat out refused to go anywhere. You check the patient out and try to convince her to go to the hospital but the patient signs the refusal. The patient’s condition deteriorates and the family takes her to the ER where a hip fracture is found. The family then sues you. This was a real court case and you can read the JEMS article here. The result was that the court decided in favor of the medics. Even though a patient has signed a power of attorney does not mean they can no longer make decisions for themselves. Document everything and follow your company’s protocols.
The legal age of a patient to make an informed decision about his health care will vary from state to state. If the patient is not old enough to make this call then until the patients legal guardian is contacted treat and transport under implied consent. One possible caveat to this is an emancipated minor.
If you are still unsure if you should be transporting a patient against his will contact a supervisor or medical control.
In my area the doctors here will not tell you it is ok not to transport the patient. Instead we use online medical control for advise in talking the patient into going to the hospital. Document this as it will add protection in court.
Tags:liability, patient care, refusal
Posted in Featured, Patient Care, slider | 4 Comments »
Recently I assisted my company in updating our protocols. One topic I covered was the patient refusal. I wanted a new perspective on the matter with the goal of decreasing the risk of litigation as well as decreasing the total number of refusals. My approach was to first see how others were tackling refusals. I researched the protocols of other services and read many articles on the topic. It was obvious that the industry standard left grey areas that needed to be addressed. I then looked to the courts to answer some of the remaining questions by researching every court case I could find where someone first refused care and later sued the provider. With the help of our medical director this information was compiled to produce our new Informed Patient Refusal Protocol. This is a multi part blog series where I will break down the important topics realized from this project.
You are dispatched to a residence for a ‘sick person’. As you arrive you enter the home after walking by 4 vehicles and multiple family members. You find the patient sitting next to a packed suitcase smoking a cigarette. The patient tells you he has had a cough for some time and wants some medicine. The patient denies SOB. You check vitals, ecg, and everything else in your assessment arsenal and only note the cough. You toss in an IV and lead a caravan of vehicles with their flashers on to the hospital.
I think everyone in EMS can relate to this and dreams of the ability to tell the patient to jump in your car and drive yourself the 1 mile to the hospital. So why don’t more services allow this? One group studied found prehospital provider refusal of transportation, as opposed to patient refusal of a transportation, accounted for 73% of the post refusal hospital admissions. Which means that to allow ground crews to determine if a patient should not be transported to the hospital would increase the risk of litigation / out of court settlement by 270%. In the future I would like to see the solution to this to be in the form of the advanced paramedic program where medics can talk to online medical control and write simple prescriptions for coughs and paper cuts but until then most services choose to take up that lovely old saying “you call, we haul”.
Tags:liability, patient care, refusal
Posted in Featured, Patient Care, slider | 3 Comments »
© Copyright 2024 | emsops.com. All rights reserved. emsops.com is proudly powered by WordPress